Monday, June 21, 2022 Wholesome Wave engaged DAISA Enterprises in 2020 to conduct a national scan of Produce Prescription Programs* to further the evidence-based and policy-change potential for investment in food & health systems through the produce prescription model. This research defines and documents the reach and complexity of programs across the country, field-wide themes, collective resources, program operator challenges, innovations, and needs across the past 10 years. Explicitly quantifying the number of programs led by Black, Indigenous, People of Color (BIPOC) was not a direct aim nor feasible within this research. However, this report, in recognition of systemic health inequities that disproportionately affect BIPOC communities and demand that opportunity and resources be dispatched, notes a growing amount of BIPOC-led produce prescription programs.

DAISA identified and researched 108 new Produce Prescription Programs which began between 2010-2020 (94 active as of December 2020) and compiled a Program Operator Database consisting of data points related to program eligibility & operations, partnership development, program longevity, prescription redemption mechanism, funding sources, and more. Research also included in-depth semi-structured interviews with 19 of the program operators and compilation and review of 93 literature and media sources including news articles, press releases, peer-reviewed academic articles, reports & policy briefs, and program implementation guides & toolkits. Through data analysis, the field scan describes the current landscape of the Produce Prescription field and lifts up the following key themes:
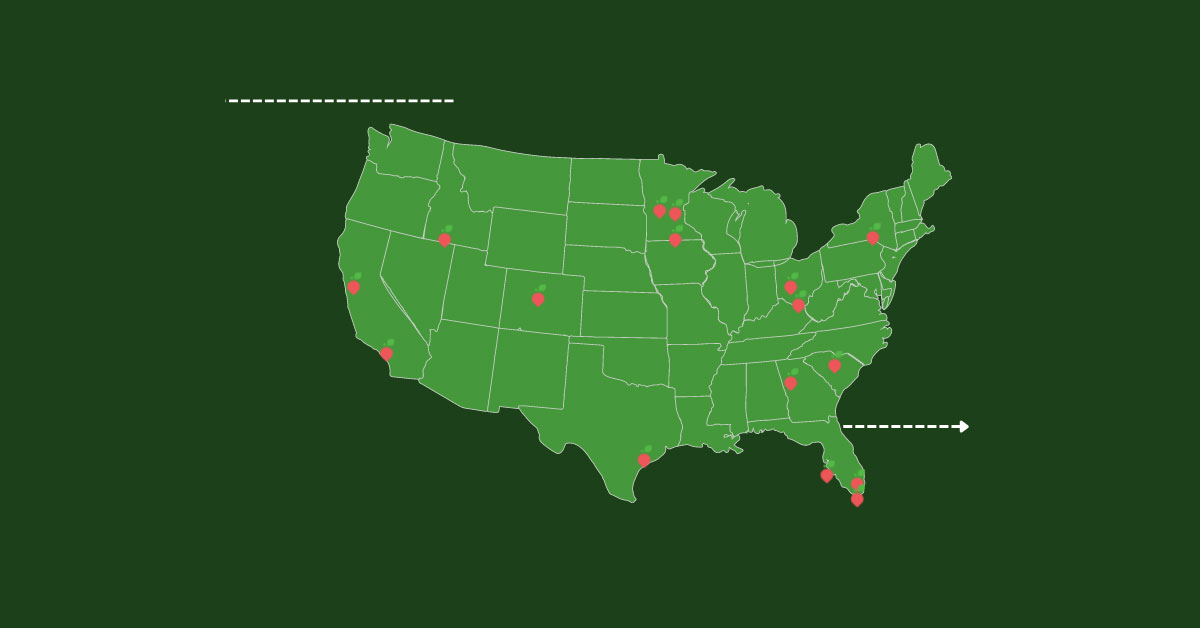
1. Geographic Distribution | Between 2010 and 2020, 108 new programs housed within or partnering with healthcare entities began operations throughout the United States, with the fastest growth occurring within the last five years. There is a fairly even distribution of programs by region: 19.8% in the south, 23.6% in the midwest, 25.5% in the northeast, and 33.1% in the west.
2. Prescription Redemption | To redeem prescriptions, 48% of programs partner with farmers’ markets, and 68% utilize a paper voucher. However, partnerships with retail grocery markets (29%) and on-site produce distribution (20%) are also gaining popularity as programs seek to diversify access.
3. Program Eligibility | The top three health factors used to screen eligible produce prescription patients were food insecurity (38%), unspecified diet-related chronic diseases (51%), and diabetes/pre-diabetes (33%). To increase equity and access, many programs are shifting away from requiring a diagnosis of a diet-related condition and instead screening more broadly for food insecurity or being at risk for disease.
4. Barriers to Participation | Programs are developing innovative models and partnerships to address prescription redemption barriers such as lack of accessible farmers’ markets and grocery stores in rural areas, access to transportation and childcare, mobility challenges, and economic & cultural differences.
5. Building Partnerships | Hospital or clinic staff “champions” who advocate for produce prescriptions as preventative care are often crucial to program initiation and success, although that can leave programs vulnerable to collapse without overall institutional buy-in.
6. Nutrition Education | 72% of programs name nutrition education or culinary instruction as a crucial component that increases prescription redemption and produce utilization in the home, indicating the effectiveness of more robust, high-touch program offerings.
7. Evaluation & Metrics | While program integration with participants’ Electronic Medical Record is not the norm, those programs with this access experience greater success with recruitment, documentation of health outcomes, and proving program effectiveness.
8. Funding Sources | Inconsistent funding leaves programs at risk of failure and hinders efforts to grow and innovate. There is a resounding call to integrate produce prescriptions as a preventative healthcare service within Medicare, Medicaid, and insurance plans.
9. Impact of COVID-19 | The pandemic has exacerbated food insecurity, especially within BIPOC communities and the need for nutrition incentives is higher than ever. In pivoting operations, some programs have increased efficiency through delivery or drive-through market models and virtual educational offerings, while acknowledging the effects of inequitable Internet access and fewer opportunities for healthy social interaction.

Recommendations: Advancing the Field
Below we provide 10 recommendations across two primary areas, Establishing & Sustaining Programs and Bolstering Research for Understanding & Advocacy, to support on-the-ground program operators and partners to continue building a robust, equitable, and sustainable Produce Prescription field.
Establishing & Sustaining Programs
1. Form an open, inclusive Produce Prescription Community of Practice or Learning Community for program operators focused on information exchange, field coordination, and mutual support among existing and emerging programs.
2. Ensure that the evolving National Produce Prescription Collaborative includes a diverse body of operators and representatives of all sectors engaged in Produce Prescription programs, with core objectives of advancing equity and policy changes.
3. Identify dedicated Produce Prescription technical assistance consultants, alongside the services available for GusNIP recipients, in order to:
a. guide emerging programs and advance or scale up program operations.
b. support hospital-based program staff who need guidance in implementing community-based programs or building relationships with local food vendors.
c. assist programs’ compliance with patient privacy laws (e.g. HIPAA) and integrating Electronic Medical Record referral technology
4. Create a public, searchable database of federal and state-level funding opportunities for Produce Prescription programs. Specifically research and compile models of state 1115 Waiver (Medicaid) funded programs and reimbursable structures to increase awareness and utilization and advocate for adoption in additional states.
5. In addition to program implementation funding, ensure designated funding is available for robust Produce Prescription program data collection and evaluation, alongside what is available for GusNIP recipients.
Bolstering Research for Understanding & Policy Advocacy
1. Advance research on the extent of Produce Prescription programs led by and for Black, Indigenous, and other People of Color (BIPOC) and recommendations to ensure a racial equity imperative is embedded within all policy and program resources.
2. Compile all current and past Produce Prescription field research into one easily accessible location.
3. Research and compile strategies and tools to support healthcare partners to increase patient recruitment and better capture healthcare cost savings. Simultaneously work also to affirm a values-based care model that not only assesses Return-on-Investment (ROI) but is inclusive of Patient-Oriented-Metrics (POM) including patient satisfaction, sense of wellbeing, social cohesion, and mental health.
4. Research and design a broadly-applicable, culturally-based nutrition education curriculum to complement the Produce Prescription program development.
5. Building upon the findings in this report and others, continue researching effective program design components including eligibility re5. Building upon the findings in this report and others, continue researching effective program design components including eligibility requirements, prescription redemption methods, dosing levels, and program duration – to better understand variations and efficacy, toward best practices. Ultimately the big promise of Produce Prescription Programs is the betterment of people’s health and well-being for whom this effective model is both a prevention tool and healthcare intervention. This research demonstrates the broad, community-driven movement to design and operate programs in various urban, suburban, tribal, local, regional and statewide formats. We must both continue to bolster all of these programs and to collectively drive to embed and institutionalize Produce Prescriptions within the healthcare payment model.